How do we hear?
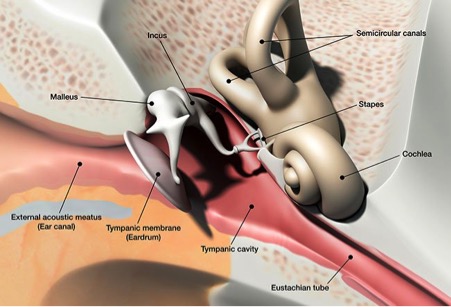
The ear consists of the outer, middle and inner ear. Sound travels through the outer ear and reaches the eardrum, causing it to vibrate. The vibration is then transmitted through three tiny bones in the middle ear called the ossicles. These three ossicles are called malleus, incus and stapes, sometimes known as hammer, anvil and stirrup. The vibration then enters the inner ear which is a snail-shaped bony structure filled with fluid. The nerve cells within the inner ear are stimulated to produce nerve signals. These nerve signals are carried to the brain, where they are interpreted as sound.
What is otosclerosis?
Otosclerosis is a disease of the bone surrounding the inner ear. It can cause hearing loss when abnormal bone forms around the stapes, reducing the sound that reaches the inner ear. This is called conductive hearing loss. Less frequently, otosclerosis can interfere with the inner ear nerve cells and affect the production of the nerve signal. This is called sensorineural hearing loss.
Who gets otosclerosis?
The cause of otosclerosis is not fully understood, although it tends to run in families and can be hereditary. People who have a family history of otosclerosis are more likely to develop the disorder. Otosclerosis affects the ears only and not other parts of the body. Both ears are usually involved in some extent. However, in some individuals, only one ear is affected. It usually begins in the teens or early twenties. Some research suggests a relationship between otosclerosis and the hormonal changes associated with pregnancy.
What are the symptoms?
The commonest symptom is hearing loss that may take many years to become obvious. The degree of hearing loss may range from slight to severe. It can be conductive, sensorineural or both.
In addition to hearing loss, some people with otosclerosis may experience tinnitus or noise in the ear. The intensity of the tinnitus is not necessarily related to the degree or type of hearing loss. Very rarely, otosclerosis may also cause dizziness.
How is otosclerosis diagnosed?
An examination by an specialist ENT surgeon is needed to rule out other diseases or health problems that may cause these same symptoms. The amount of hearing loss and whether it is conductive or sensorineural can be determined only by careful hearing tests. Your otolaryngologist may order a CT scan of the ear to assess the extent of otosclerosis.
How can otosclerosis be treated?
There is no known cure for otosclerosis. The individual with otosclerosis has several options: do nothing, be fitted with hearing aids, or surgery. No treatment is needed if the hearing impairment is mild.
Hearing aids amplify sounds so that the user can hear better. The advantage of hearing aids is that they carry no risk to the patient. Your specialist can discuss the various types of hearing aids available and make a recommendation based on the specific needs of an individual.
Aims of the proposed treatment
If one ear is affected, the operation may help to locate the direction of sound and hear better in noisy background.
If both ears are affected, the operation is usually done on the poorer ear. The patient may still need a hearing aid in the opposite ear.
You may change your mind about the operation at any time, and signing a consent form does not mean that you have to have the operation.
If you would like to have a second opinion about the treatment, you can ask your specialist. He or she will not mind arranging this for you. You may wish to ask your own GP to arrange a second opinion with another specialist.
How is the operation done?
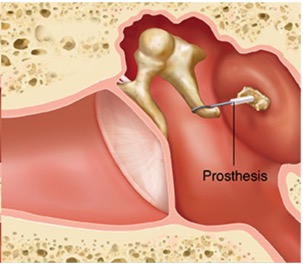
The operation is called stapedotomy and usually takes about an hour. You might be asleep although some surgeons prefer to do the operation with only your ear anaesthetised so that they can monitor your hearing during the operation. Your surgeon should consult you before making such decision. A cut is made above the ear opening or inside the ear canal. The top part of the stapes is removed with fine instruments. A small opening is then made at the base, or “footplate”, of the stapes into the inner ear. Some surgeons use laser to perform this procedure but it is not essential.
A small piece of vein may be taken from the back of the hand to use as a graft inside the ear. It will not cause permanent harm to the hand. A plastic or metal prosthesis is then put into the ear to conduct sound from the remaining ossicles into the inner ear. You will have packing placed in the ear canal. All modern metal prostheses are not affected by MRI scan or airport scanner, should you need one in the future.
How successful is the operation?
The chances of obtaining a good result from this operation by experienced surgeons are over 80 percent. This means that eight out of ten patients will get an improvement of hearing up to the level at which their inner ear is capable of hearing. You should enquire from your surgeon his/her personal success rate of stapedotomy. Many surgeons keep a database of their results.
Possible complications
There are some risks that you must consider before giving consent to this treatment. These potential complications are rare. You should consult your surgeon about his complication rate.
Loss of hearing:
In a small number of patients the hearing may be further impaired due to damage to the inner ear. It can even result in a severe loss of hearing in the operated ear. This may be to the extent that one cannot obtain benefit from a hearing aid in that ear. For experienced surgeons, this complication happens in around one in 100 patients. Therefore the poorer hearing ear is normally selected for surgery first.
Dizziness:
Dizziness is common for a few hours following stapedotomy and may result in nausea and vomiting. Some unsteadiness can occur during the first few days following surgery; dizziness on quick head movement may persist for several weeks. On rare occasions, dizziness is prolonged.
Taste disturbance:
The taste nerve runs close to the eardrum and may occasionally be damaged. This can cause an abnormal taste on one side of the tongue. This is usually temporary but it can be permanent in one in ten patients.
Tinnitus:
Sometimes the patient may notice noise in the ear, in particular if the hearing loss worsens. The uncommon risk of total loss of hearing, disturbance of balance or taste could have a serious implication to certain employments. You should discuss with your specialist about these concerns. Some specialists also advise against scuba diving, sky diving or use of firearm following a stapedotomy operation.
Does it hurt?
The ear may ache a little but this can be controlled with painkillers provided by the hospital.
What happens after the operation
You will usually go home the day after the operation or sometimes the same day. A slight amount of dizziness is normal after the operation. The stitches will be removed one to two weeks after the operation. There may be a small amount of discharge from the ear canal. This usually comes from the ear dressings. The packing in the ear canal will be removed after two or three weeks.
You should keep the ear dry for the first few weeks. Plug the ear with a cotton wool ball coated with Vaseline when you are having a shower or washing your hair. Avoid straining for the first few weeks after surgery, that is, no heavy lifting. Only blow the nose gently. Avoid air travel until cleared by your surgeon. Hearing may not return to normal for up to three months. You should consult the surgeon if there is a sudden onset of deafness, dizziness or severe pain after you are discharged from the hospital. You are advised to avoid diving or flying when you have a cold if possible.